The Agrofood Industry and Its Political Activities
12 December 2021
Health and Politics
12 December 2021By Catherine Cavalin, IRISSO & LIEPP, and Paul-André Rosental, Centre for History
Scope and Discussion of the Epidemiological Transition
For half a century, the so-called epidemiological transition model has guided the interpretation of mortality data. Based on long-term trends in morbidity, it focuses on declining mortality from communicable diseases and the rise of non-communicable chronic diseases (primarily cancer and cardiovascular diseases). In this model, the lower incidence of diseases that can be controlled by vaccination and medication (especially antibiotics) is counterbalanced by the increase in diseases related to living conditions (e.g. pollution, nutrition, sedentary lifestyle). The two phenomena are linked: since infectious mortality has long massively impacted children and young people, its reduction is a factor in population ageing, which in turn increases the frequency of chronic diseases associated with age.
This paradigm has seen many refutations, due to local situations (in South Africa, for example, where widespread tuberculosis and HIV-AIDS infections coexist with non-communicable diseases such as silicosis in the mining sector and cardiovascular diseases) or to temporary epidemic outbreaks (Ebola, SARS). But the epidemiological transition is still used to interpret global epidemiological data. Until the advent of covid19, no known or emerging infectious disease had challenged the trend advanced by this ‘transition’ model as much as the new coronavirus.
Covid19 definitively felled the two premises supporting this model. The first was confidence in the ability to rapidly develop cures or vaccines in the event of a serious infectious outbreak. The second was the belief, based on the precedent of HIV-AIDS in the 1980s, that no new infectious agent would scale up into a global pandemic capable of decimating populations. The preparedness plan that the World Health Organization (WHO) recommended in 1999 did not challenge this view(1)World Health Organization, Influenza pandemic preparedness plan: the role of WHO and guidelines for national and regional planning, 1999.. Granted, after the warning shot of the H5N1 influenza subtype (Hong Kong, 1997), it did not exclude the possibility of a large-scale pandemic, with significant containment measures in the event that a vaccine response lasted more than a year. But it focused on preventing severe influenza outbreaks. And the plan also followed a public health communication approach aiming at avoiding the panics caused by ‘false alarms’ since the 1970s. The limited scale of the H5N1 avian flu epidemic in 2004 and H1N1 in 2009 left this view unchallenged. .

Présentation de la stratégie innovation santé 2030 par le Président Emmanuel Macron. Juin 2021. Source : Élysée
By contrast, 18 months into the covid19 pandemic, Emmanuel Macron’s announcement of the Health Innovation Strategy 2030, wherein 750 million euros was allocated to combating infectious diseases (out of an unprecedented 7 billion euros of funding focused on three priorities), appears to challenge the epidemiological transition model. The question we ask is whether this reorientation addresses contemporary medical problems that were prevalent when covid19 emerged, and that have evolved since. We also hope that our answer will shed light on how two social scientists can opine on this issue not only as observers of ‘what is happening in medicine’, but also as actors working and publishing in close collaboration with medical teams(2)The co authors also contributed, among others, to the publication of « Beyond silicosis, is the world failing on silica hazards? », The Lancet Respiratory Medicine , 2029; « The nosology of systemic sclerosis: how lessons from the past offer new challenges in reframing an idiopathic rheumatological disorder », The Lancet Rheumatology, 2019 ; « Paediatric sarcoidosis », Paediatric Respiratory Reviews, 2018 ; « Silica-associated Systemic Sclerosis in 2017: Sixty years after Erasmus, where do we stand? », Clinical Rheumatology, 2017..
Abdel Omran, an Egyptian public health specialist at the WHO, formulated the epidemiological transition model in 1971(3)Abdel Omran, “The Epidemiologic Transition: A Theory of the Epidemiology of Population Change”, Milbank Mem. Fund. Q., 1971.. He had just transposed the post-war ‘demographic transition’ model onto the public health field(4)Simon Szreter, “The Idea of Demographic Transition and the Study of Fertility Change: A Critical Intellectual History”, Population and Development Review, 1993.. A 2009 article(5)George Weisz, Jesse Olszynko-Gryn, « The Theory of Epidemiologic Transition: the Origins of a Citation Classic », Journal of the History of Medicine and Allied Sciences, 2009. showed that this transposition helped rebalance health policies (and therefore the role of the WHO) in relation to demographic policies. The latter, which rose to prominence in the 1960s in the form of massive fertility reduction policies in developing countries (in a way of fulfilling the predictions of the demographic transition model), had boosted the organisations carrying them out: UN agencies, large American foundations, and national and transnational NGOs(6)Matthew Connelly, Fatal Misconception: The Struggle to Control World Population, Harvard University Press, 2008..
The Global Burden of Disease as the Epitome of the Epidemiological Transition?
In the 1990s, the Global Burden of Disease (GBD) came to both epitomise and promote the global validity of the epidemiological transition model. Originally conceived by the World Bank, this publication has been produced since 1998 by the WHO’s Disease Burden Unit, and since 2007 by the Institute for Health Metrics and Evaluation. Based at the University of Washington in Seattle, its backers include the Bill & Melinda Gates Foundation, and it draws on an international network of thousands of researchers. The GBD currently provides detailed morbidity, disability, and mortality data for more than 200 countries and hundreds of diseases and causes of injury(7)Ce paragraphe s’appuie sur : GBD History. Voir aussi : Conrad Keating, « The Genesis of the Global Burden of Disease Study », The Lancet, 2018..
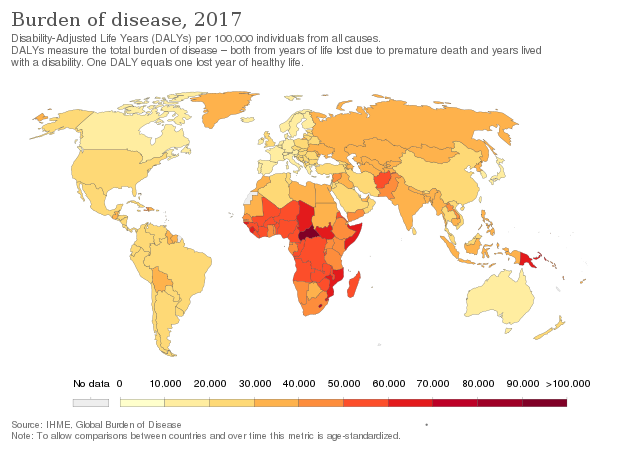
The GBD uses DALYs (disability-adjusted life years) as a measure of years of life lost from premature death (YLL) and years of life lived in ill health and disability (YLD). These three measures – DALY, YLL, and YLD – are used to produce statistics based on the divide between communicable and non-communicable diseases. As aforementioned, the GBD thus epitomises the epidemiological transition model and the divide it posits between these two categories of diseases.
The various GBD measures do indeed support, in absolute numbers, the quantitative decline of communicable diseases in relation to non-communicable ones(8)GBD 2013 DALYs and HALE Collaborators et al., Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition, The Lancet, 2015.. But the introduction of demography complicates this trend. If we reason in terms of rates per 100,000 people, the fall of DALYs is certainly accelerating for communicable diseases, but it is stagnating for chronic diseases. More disconcertingly, the number of DALYs is falling for both types of disease if we neutralise the effect of population ageing. Statistically, based on a population of standardised ages, the decline in chronic morbidity rates is almost as rapid as the decline in infectious morbidity rates, with both declines accelerating in the 21st century.
These data predate the advent of covid19, and it is unknown to what extent it will depress (rather than the reverse) the decline in DALYs related to communicable diseases. Already challenged by demography, the epidemiological transition model has also been challenged by medicine and epidemiology since before the pandemic – and even more so since.
The lesson from the effects of covid19 is indeed far from simply portending a return to the ‘raw’ danger of infectious diseases. This is precisely the issue raised by Emmanuel Macron’s launch of a public health investment program. It is worth explaining some key takeaways, in conclusion.
Is Covid19 (only) a Communicable Disease?
One of the striking epidemiological features of the covid19 pandemic is the unequal social distribution of the disease’s incidence and severity. This alone suggests that the ‘communicable’ descriptor used for covid19 should give pause.

Shutterstock
While the communicable SARS-CoV-2 is a causal agent of covid19, the social inequalities in exposure to the disease and its most severe forms indicate that noncommunicable factors play a determining role in the epidemiology of the disease. While this mix between the infectious and environmental (social) determinants of covid19 seemed to reveal social inequalities in health throughout the pandemic in an unprecedented way, there have long been many reasons to make the connection. Pasteur himself (and pasteurism) has often been caricatured as proponents of the reductive causal logic of ‘one germ, one disease’, which suggests the necessity and sufficiency of an infectious agent in the manifestations of a communicable disease. However, as early as in Pasteur’s work, the causality of an infectious agent leading to an associated disease was conceived with an environmental approach, with strong variations attributable to the environmental conditions in which the contagion occurred(9) J. Andrew Mendelsohn, “‘Like All That Lives’: Biology, Medicine and Bacteria in the Age of Pasteur and Koch”, History and Philosophy of the Life Sciences, 2002.. Recent, pre-covid19 debates in epidemiology and medicine were also moving in this direction, as seen in reflections around nosology – the discipline that studies diseases in order to classify them – and the attendant naming conventions. To take just two examples, the notion of syndemic(10)Merrill Charles Singer et al., “Syndemics and the biosocial conception of health”, The Lancet, 2017; Richard Horton, “COVID-19 is not a pandemic”, The Lancet, 2020.refers to synergies between diseases (both communicable and not) and socio-environmental conditions, while the idea of a ‘socially transmissible (11)Luke N. Allen, Andrea B. Feigl, “Reframing non-communicable diseases as socially transmitted conditions”, The Lancet Global Health, 2017; Catherine Cavalin, Alain Lescoat, “From (re-)framing NCDs to shaping public health policies on NCDs and communicable diseases”, The Lancet, 2017; Catherine Cavalin, Alain Lescoat, Odile Macchi, Matthieu Revest, Paul-André Rosental, Patrick Jégo, “Reframing noncommunicable Diseases”, The Lancet Global Health, 2017. disease has been discussed as a lever to rethink the nosological boundary between communicable and noncommunicable.
These blurred boundaries give the social sciences an active role in and with medical research, understood in its clinical and epidemiological aspects. By overlaying the immediacy of infectious contagion with the long duration of living conditions, and by highlighting professional and environmental risk factors in the lives of individuals, they show that it behooves medicine to seek the know-how of the social sciences in order to reconstitute life trajectories through anamnesis. The results thus obtained for chronic systemic diseases similar to covid19 in their effects and immune mechanisms(12)Catherine Cavalin, Mickaël Catinon, Odile Macchi, Michel Vincent et Paul-André Rosental, « Expositions aux particules inorganiques : comment poser la question ? » in Emmanuelle, Mercklé Pierre (dir.), Un panel français. L’Étude longitudinale par internet pour les sciences sociales (ELIPSS), 2021., provide, we hope, promising cases in point.
Paul-André Rosental is a University Professor at the Sciences Po Center for History (CHSP) and a member of the Council of Advisors of the Population European research network. His research covers the whole biopolitical field, from demography and population policies to public health and welfare. He also studies occupational diseases, and the role of socio-environmental factors in the triggering of some chronic diseases. Catherine Cavalin is a sociologist and CNRS research fellow at the Institute for Interdisciplinary Research in Social Sciences (IRISSO, Paris-Dauphine, PSL). She was previously a researcher at the Center for European Studies at Sciences Po, as part of the SILICOSIS research project funded by the European Research Council (ERC) and led by Paul-André Rosental. She is also an associate researcher at the Center for Employment and Labor Studies (CEET, CNAM) and the Laboratory for Interdisciplinary Evaluation of Public Policies (LIEPP) at Sciences Po.
Notes